- Make It Yourself Lavender Heart-Shaped Bath Bombs!
- 20 Things You Never Knew About “Down There”
- 12 Best Foods For Those Suffering From Arthritis Pain
- 12 Personal Hygiene Mistakes Almost Everyone Makes (Mom Never Told You About #4!)
- 15 Medicinal Plants And Herbs From The Cherokee People
- 12 Mind-Blowing Benefits Of Drinking Coconut Water During Pregnancy
- 12 Outstanding Winter Foods That Won’t Fatten You Up Like A Christmas Turkey
Treat Your Seasonal Allergies Naturally!

Photo credit: bigstock.com
If you’re one of the 36 million Americans battling seasonal allergies, the leaves won’t be the only things changing. Runny noses, itchy throats, and incessant sneezing can put a damper on an otherwise lively time as the holiday season approaches, but the misery doesn’t have to last long. Though over-the-counter antihistamines such as Benadryl offer temporary relief from seasonal allergies, natural remedies can safely reduce symptoms without side effects.
1. Ginger
Ginger has long been touted for its anti-inflammatory effects in the human body. The body’s immune response includes mobilizing molecules called pro-inflammatory cytokines, which are responsible for inducing inflammation in affected sites. Allergies are essentially instances when the immune system abberently responds to foreign matter that’s usually regarded as harmless. This response leads to inflammation, specifically that of the throat and internal areas of the nose. Studies show that ginger minimizes such inflammation and provides those suffering from allergies with much-needed relief. A Japanese study using mice demonstrated that ginger extract reduced sneezing intensity and runny noses in subjects by reducing the secretion of the antibodies responsible for seasonal allergies. Peppering meals with ground ginger or enjoying freshly carved ginger in one’s morning tea can produce similar defenses against the effects of allergies.
2. Probiotics
Most view their gut solely as the center of digestion, but this evolved system is so complex and central to our functioning that it’s often referred to as “the second brain”. Over half of the body’s immune system is constrained to the gut, so a strong defense against infection and abnormal immune reaction relies on gut health. As allergies can be categorized as abnormal immune reactions, it’s unsurprising that they are impacted by the condition of the gut, or that probiotic usage can mitigate the misery accompanying seasonal allergies.
A Japanese double-blind, placebo-controlled trial analyzed the impact of probiotics on forty subjects suffering from cedar pollinosis, a form of spring rhinitis equivalent to seasonal allergies. The condition, according to self-reported questionnaires, affects almost a third of Japanese residents. Each member of the trial was made to regularly consume either yogurt rich in a strain of probiotic bacteria called Bifidobacterium longum BB536 or a placebo substitute. Those who consumed the bacteria-saturated yoghurt experienced reduced nasal blockage and irritation, along with attenuated throat symptoms.
A second randomized trial, this one on nearly 50 patients suffering from seasonal allergies, administered a probiotic-rich milk containing a strain of bacteria called Lactobacillus acidophilus strain L-92 or a placebo. After the trial period ended, researchers noted that trial subjects issued the probiotic-infused milk had reduced instances of watery, itchy eyes, nasal leakage, and nasal swelling. Yet a third experiment demonstrated that probiotics can reduce the magnitude of IgE antibodies (an antibody produced in response to typical seasonal allergens) and inflammatory cytokines that the body manufactures in response to allergen encounters.
Continue to Page 2
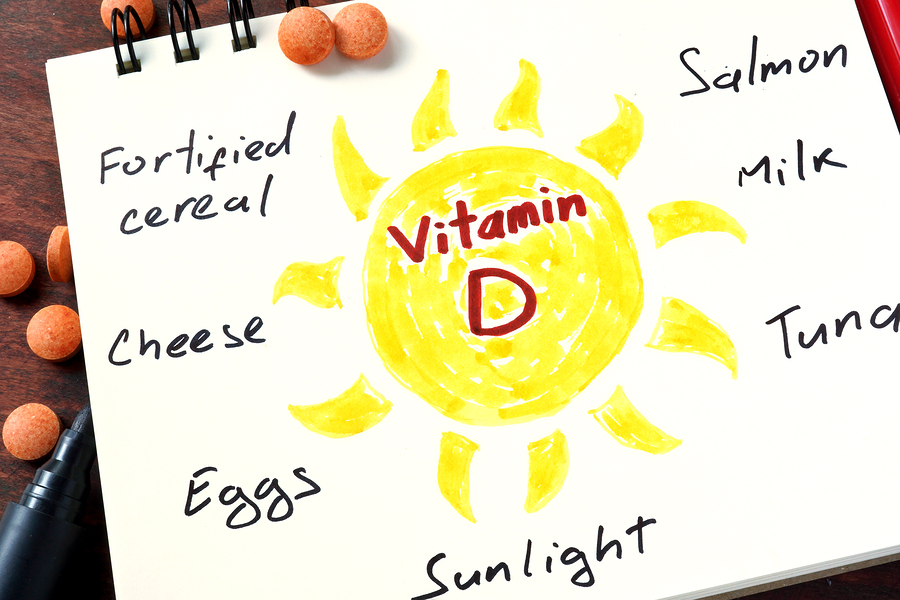
Photo credit: bigstock.com
3. Vitamin D
A correlation between Vitamin D deficiencies and respiratory ailments has been observed, making it reasonable to expect that a relationship between insufficient intake of this vitamin and seasonal allergies and asthma would also be observed. One study took nearly 1,000 asthmatic juvenile subjects and conducted serum 25-hydroxyvitamin D tests (which convey the body’s entire vitamin D reserve). It was observed that eczema, asthma, and allergy-based rhinitis were significantly higher amongst children suffering from vitamin D deficiencies. IgE marker testing further revealed that children with lower vitamin D scores produced more IgE. Again, IgE is an antibody the immune system generates in response to allergy-inducing materials.
Another study examined the synergistic effects of vitamin D and probiotics on children affected by allergic rhinitis and those who indicated sensitivity to grass pollen. During this randomized, placebo-controlled trial, children were issued either probiotics and vitamin D supplements or placebo equivalents. Members of the former group experienced a reduction in allergy symptoms.
4. Pycnogenol
When oxygen reacts with other compounds in the body, uncharged, highly reactive molecules called free radicals are often generated. Free radicals are believed to play a role in the pathology of everything from accelerated aging to cancer, but research has shown they’re also involved in discharging histamine from the body’s mast cells, which are white blood cells involved in immune response. Histamine is responsible for the scratchy throat, itchy eyes, and leaking nose that burdens sufferers of seasonal allergies, and most anti-allergy medications work by inhibiting its production. Pycnogenol, derived from the French maritime pine tree, is efficient at eliminating free radicals. The relationship between pycnogenol and free radicals led to researchers studying whether the pine extract could mitigate allergy symptoms. A double-blind, placebo-controlled trial found that pycnogenol did indeed lessen histamine production as anticipated, and consequently the patients’ allergic responses as well.
A second placebo-controlled study examining the effects of pycnogenol on rhinitis gathered 39 subjects who routinely contracted allergy symptoms at the onset of allergy season. The patients were split into two groups, one of which was supplemented with pycnogenol for five to eight months before birch allergy season began. Not only did this group experience reduced allergy symptoms in comparison to those who had received the placebo, but their IgE antibody output for birch pollen increased by 19.4%, while the placebo group comparatively experienced a 31.9% increase of the same. Researchers further inferred that the sooner patients began pycnogenol supplementation before the allergy season began, the more it offered protection.
Continue to Page 3

Photo credit: bigstock.com
5. Bee Medicine
As if nature’s tiny golden workers do not already provide enough mankind with enough resources, it has become clear that consuming bee products drastically reduces allergic response. A 2011 study reported in the Archives of Allergy and Immunology demonstrated preseasonal consumption of birch pollen honey reduces allergy symptoms by 60% and antihistamine usage by 50% in comparison to those who do not regularly consume birch pollen honey, propolis, or other bee products.
A fallacious explanation for why honey effectively combats allergy symptoms has permeated health groups and the general population to no small extent. The erroneous rationale claims that bee products work similarly to vaccines. By repeatedly exposing the body to honey and, supposedly, bee pollen, the immune system builds up a tolerance for the pollens consumed. There is not ample evidence supporting this logic. Honey contains very little pollen, not nearly enough to provide the claimed value; bees do not use it in the honey manufacturing process. Furthermore, most allergies are rooted in grasses and weeds, not the vibrant flowering plants that blossom each allergy season, from which bees procure their nectar.
READ ALSO: 8 Food-Remedies For Allergy Infographic
Studies suggest bees’ allergy-busting attributes lie in a compound called myricetin that reduces histamine production.
References:

































